IUD's
IUD insertions and removals are available at Glebe Hill Family Practice with Dr Anna Kingshott or Dr Victoria Whelan and at GHFP Nurture with Dr Isabel Pemble or Dr Heather Price.
IUDs are used for long-term contraception, and can be helpful for women with bleeding problems.
What is an IUD?
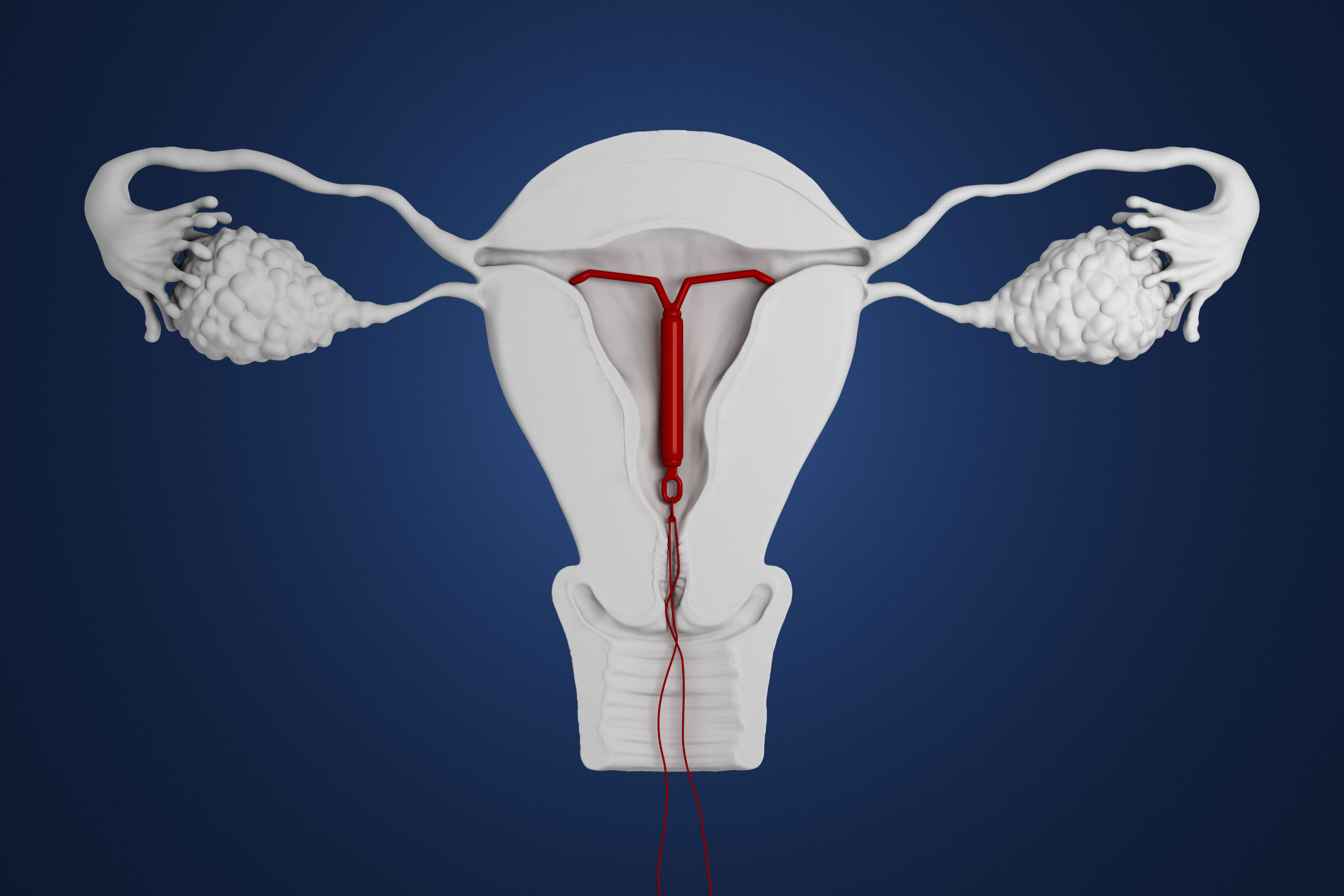
An Intrauterine Device (IUD) is a form of contraception that is placed in the uterus. There are two types of IUD’s available in Australia:
Mirena IUD's– a hormonal IUD made of plastic and containing a synthetic form of progesterone (a female hormone) which is slowly released into the uterus;
Copper IUD’s – an IUD made of plastic and copper
How do IUD’s work?
Both copper and Mirena IUD’s:
- Work by the main action of prevention of fertilization by stopping sperm from moving up to the fallopian tubes and slowing the movement of eggs through the fallopian tubes.
- They also change the lining of the uterus to make it hostile to a fertilized egg and prevent implantation (it is very rare for an egg to be fertilized).
The Mirena also thickens cervical mucous preventing sperm from entering the uterus and sometimes prevents or delays ovulation (the release of an egg) each month – especially in the first 3 months of IUD use.
When does it start working?
- The copper IUD is effective immediately (as long as pregnancy is first excluded).
- The Mirena is effective immediately if inserted in the first 7 days of the menstrual cycle, otherwise it takes 7 days to become effective.
Benefits of IUD’s
- Highly effective, inexpensive, easily removed
- They work for 5-10 years, depending on the type
- Once inserted, you only need to remember to check the string each month (compared to remembering a pill every day…)
- Once removed fertility rapidly returns to your normal level
- They are safe during breast feeding
- Their effectiveness is not reduced by other medications or illness such as diarrhea and vomiting
- They are usually safe options if you are unable to take contraception containing oestrogen
- Copper IUD’s can be used by women who cannot use any hormonal contraception or prefer a non-hormonal method
- The Mirena usually reduces the amount of menstrual flow by 80-90% and is ideal for women with heavy periods. 20% of women stop getting periods completely.
Disadvantages of IUD’s
- They can only be inserted by a specially trained doctor.
- Insertion can be uncomfortable. This is helped by use of local anaesthetic. The insertion may be more uncomfortable if you haven’t had children.
- There may be complications at the time of insertion (see below).
- They do not protect you against sexually transmitted infections (STI’s), and are not recommended for women who are at very high risk of STI’s. Use condoms to protect yourself against STI’s, especially with new sexual partners.
- Periods tend to be longer, heavier and more painful. On average bleeding is increased by 20-50% (roughly 1-2 tablespoons per month for most women). The bleeding may settle with time.
- Copper IUD’s are not on the PBS. The usual cost of the IUD is about $160. They must be ordered from specialist medical suppliers and there may be a delay in availability.
- When first inserted there tends to be frequent light bleeding which usually settles within 3 months.
- There may be hormonal side effects – headache, acne, breast tenderness, mood change – these are uncommon and usually improve with time.
- Women who have had actice breast cancer within the last 5 years should not use the hormonal IUD.
Complications
- There is a very small risk (<1 in 1000) of puncturing the wall of the uterus during insertion (perforation). The IUD may then pass through the wall of the uterus and require surgical removal. This risk is greatest in women who are breast-feeding or have delivered recently.
- There is a very small risk of infection occurring in the first 3 weeks after insertion. A pelvic infection can lead to damage to the fallopian tubes affecting fertility.
- The IUD may be expelled (fall out) from the uterus. This is most common in the first 3 months and usually happens during a period. It may occur without the woman knowing. We recommend checking for the strings monthly.
- There may be an increase in vaginal discharge.
- Although the failure rate is very low, it is important to see a doctor as soon as possible if you think you may be pregnant as IUD’s can harm the outcome of a pregnancy. About 1 in 20 IUD pregnancies form in the fallopian tubes (ectopic pregnancy). There is also increased risk of infection, late miscarriage and prematurity if the pregnancy continues and the IUD can’t be removed.
If you wish to have an IUD inserted at our practices
Advise our reception staff who will book you in for a half hour pre-insertion (assessment) appointment with Dr Anna Kingshott, Dr Victoria Whelan (Glebe Hill Family Practice), Dr Isabel Pemble, Dr Heather Price (GHFP Nurture).
You will be given information and asked questions by the doctor to ensure the IUD is appropriate for you. You will also be examined and offered any necessary investigations (sometimes, but not always involves a pap smear and swabs).
The procedure will be explained and insertion appointment arranged. Written pre-procedure information and a prescription for your IUD will be provided at the assessment appointment.
A follow-up appointment 6 weeks after the insertion is recommended.
IUD Fees
Long GP consultation fees apply for IUD Assessment or Removal appointments prior to scheduling the IUD Insertion procedure. Information about GP consultation fees can be found here: Fees.
At the IUD Insertion appointment the practitioner will charge a private fee for the procedure, and a Medicare Rebate is applicable. There is an additional IUD Procedure Fee on the day which covers the practice's costs (consumables including disposable instruments and local anaesthetic).
Payment is required on the day of each appointment.